Cervical Screening Test
Cervical screening tests (CST) detect cervical changes to prevent cervical cancer. Obtaining a CST is exactly the same as for a PAP smear but the cells obtained are sent to the laboratory in a liquid and tested for high-risk Human Papilloma Virus (HPV) strains. If one or more of these strains are detected, the specimen is then also examined under a microscope for cellular changes. (With a PAP smear the specimen is examined under the microscope for cellular changes but an HPV test is not done.)
Below is current advice from the Department of Health:
Who should have a Cervical Screening Test?
You are eligible for a subsidised Cervical Screening Test if you
- aged between 25 and 74
- sexually active or ever have been
- a woman or person with a cervix
It makes no difference if you:
- are gay, lesbian, bisexual, transgender or straight
- have had the HPV vaccination or not
- are no longer sexually active
- have been through menopause
- have only been with one sexual partner
- have experienced traditional cutting or circumcision
- have had a baby
- are pregnant (ensure to let your health care professional know)
If you have had a full or partial hysterectomy, please check with your doctor about screening.
You are eligible to have your first test when you turn 25 or 2 years after your last PAP test. Cervical screening occurs every 5 years after that in low risk women.
If you're outside the target age range
Under 25:
Routine screening starts at age 25. This is because there are common infections or abnormalities that usually go away by themselves before age 25. Cervical cancer is rare in this age group. Screening from age 25 means that we avoid unnecessary tests and treatment.
Women who already had an abnormal result should follow medical advice.
75 or over:
If you’re 75 or over you can still ask to have a subsidised Cervical Screening Test – talk to your doctor, nurse or health worker.
Talk to your doctor, nurse or health worker
See your doctor, nurse or health worker as soon as possible if you:
- have abnormal vaginal bleeding or unusual discharge
- experience pain during sex
- have an unexplained, persistent vaginal discharge.
Getting a CST done
Before your appointment
When you book an appointment, tell the receptionist if you:
- would prefer to see a female health worker
- have a disability which means you need extra support to do the Cervical Screening Test
- need the help of an interpreter during your appointment.
At your appointment
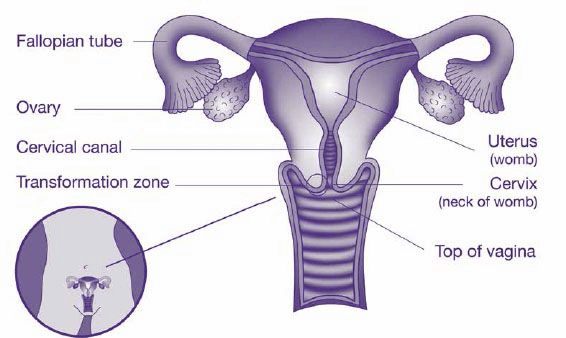
You can take a relative or friend with you to your appointment. You will be in a private space with your doctor and with a female chaperone present for male doctors. If you are unsure what to expect or is worried, talk about the process first. Usually, you will be asked to take off your clothes below the waist. You lie on your back, with knees apart. A sheet will be given to you to cover yourself. The doctor or nurse will gently insert a speculum into the vagina and a cell sample is take from the cervix with a brush. These examinations are uncomfortable but should not be painful. If it hurts, tell your doctor straight away.
The test will take less than a minute.
After the appointment
The sample is sent to a laboratory and the results usually take 1-2 weeks. A copy of the results will be sent to your GP and to the national register unless you have opted out. You can call us in 2 weeks for the results. If your results are ABNORMAL we shall call you. For most women, if the results are negative (no HPV found), you will be advised to do the test again in 5 years.
Results needing more tests
Unsatisfactory test result
This means the laboratory cannot read your sample. You will need to come back for a repeat Cervical Screening Test in 6 to 12 weeks.
An unsatisfactory result does not mean that anything is wrong, it just means the laboratory could not read the test properly for a variety of reasons. For instance if there were not enough cells collected.
Return to screen in 12 months
This means you tested positive for HPV but do not need further investigation at this time. You need to have another test in a year. There is a good chance that your body's immune system will get rid of the HPV in that time.
If the HPV infection is gone when you are retested, you will return to 5-yearly screening. If it is still there, you need a colposcopy.
If you are referred to a specialist
It means your results show either:
- that you tested positive for a type of HPV that needs further investigation
- the test found abnormal cells that may need treatment.
You will usually be referred to us for a
colposcopy. It is very important to attend this appointment for further investigation. This does not mean you have cervical cancer.
Remember that HPV infections do not usually turn into cervical cancer but because a small percentage do, we need to follow it up and sometimes treat it. Fortunately it takes a very long time from initial HPV infection to cervical cancer (around 10 years).
Recording results
The National Cancer Screening Register collects and monitors information about your screening, including test results. The register's privacy statement outlines how they handle this information.
The register sends invitations and reminders when you are due for your next Cervical Screening Test. This provides a safety net in addition to your GP and makes it easy for you to manage your participation.